

The Mullerian ducts grow caudally using the Wolffian ducts as guides. Additionally, the Wolffian duct induces the development of the Mullerian ducts from the coelomic epithelium of the paired urogenital ridges. The Wolffian duct develops from the paired urogenital ridges and grows caudally to induce the formation of the mesonephric tubules. The Wolffian ducts (mesonephric ducts) and Mullerian ducts (paramesonephric ducts) are the two main ductal systems that give rise to specific structures in the male and female genital and urinary tracts. Because pediatricians, gynecologists, and pediatric urologists encounter this diagnosis in their practice, a multi-disciplinary approach to evaluation and treatment is optimal for the patient.ĭuring urogenital development, the cloaca is divided by the urorectal septum to separate the ventral urogenital sinus from the dorsal anal canal. Surgical treatment focuses on the prevention of recurrence of the imperforate hymen. Corrective hymenectomy may be delayed until puberty unless the child suffers from urgent complications of the pelvic mass, prompting emergent surgery to preserve renal function, treat an infection, or minimize infertility. This mass may cause mechanical obstruction of the urinary tract, leading to urinary retention, hydronephrosis, or acute renal injury. Hematocolpos or hematometra, the accumulation of menstrual blood in the vaginal or uterine cavities, can create a pelvic mass identified on physical exam as a blue, bulging perineal mass. Many patients remain asymptomatic until menarche when they present with cyclic abdominal pain and amenorrhea. Infants with an imperforate hymen may develop a mucocele from endogenous maternal estrogen stimulation. An imperforate hymen can present with obstructive symptoms of the female genital and urinary tract during the perinatal, pediatric, or adolescent years and is a rare cause of primary amenorrhea. When the hymen does not spontaneously rupture during neonatal development, it is referred to as an imperforate hymen. Follow-up doses should be administered one to two and four to six months after the first dose.The hymen is a thin membrane of stratified squamous epithelium circumscribing the vaginal introitus. Postexposure hepatitis B vaccination (without hepatitis B immunoglobulin) should also be offered at the time of the initial examination if the child has never been immunized. 16 Because nausea is a common side effect, antiemetics may also be prescribed. Prophylactic treatment must be started within 72 hours of the assault with two tablets of emergency contraceptive pills (Ovral or Preven) given immediately and two tablets given 12 hours later.

15 (pp49–75) Following acute sexual assault, pregnancy prophylaxis should be offered to adolescent girls after an informed consent has been obtained and urine pregnancy test results are negative. Prophylactic antibiotics for the treatment of gonorrhea, Chlamydia, trichomonas and bacterial vaginosis should be given to sexually active adolescents following an acute sexual assault ( Table 3).
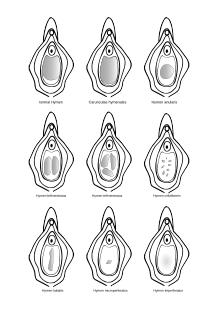
Referral for psychologic services is important because victims of abuse are more likely to have depression, anxiety disorders, behavioral problems and post-traumatic stress disorder.Īntimicrobial therapy should be initiated in prepubertal children based on the results of laboratory testing. Forensic evidence collection is indicated in certain cases. Judicious use of laboratory tests, along with appropriate therapy, should be individually tailored. When examining the child's genitalia, it is important that the physician be familiar with normal variants, nonspecific changes and diagnostic signs of sexual abuse. A careful history should be obtained and a thorough physical examination should be performed with documentation of all findings. The child's history as obtained by the physician may be admitted as evidence in court trials therefore, complete documentation of questions and answers is critical. Because the examination findings of most child victims of sexual abuse are within normal limits or are nonspecific, the child's statements are extremely important. Behavioral changes may involve sexual acting out, aggression, depression, eating disturbances and regression. Child victims of sexual abuse may present with physical findings that can include anogenital problems, enuresis or encopresis.


 0 kommentar(er)
0 kommentar(er)
